The prevalence of type 2 diabetes is increasing in the United States according to Dr. Steven Reisman, Director of the New York Cardiac Diagnostic Center and a cardiologist in New York City. Pre-diabetes is usually defined as an elevation of fasting or postprandial glucose levels. The American Diabetes Association has defined impaired fasting glucose as a level of 100 to 125 mg/dl. Also, an elevation in hemoglobin A1c or glycosylated hemoglobin (HbA1c) at a level of 5.7% to 6.4% may also represent pre-diabetes.
Metabolic Syndrome is related to pre-diabetes. Metabolic Syndrome is defined as any three of the following five components. These components include:
- an elevated glucose level
- abdominal obesity
- elevated blood pressure
- elevated triglycerides
- reduced high-density lipoprotein (HDL) cholesterol
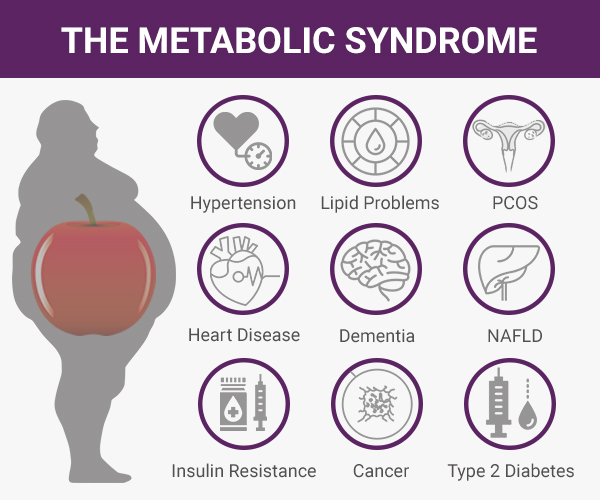
Most individuals with metabolic syndrome have abdominal obesity. It is felt that insulin resistance may be mediating the metabolic risk factors of the metabolic syndrome. Most people with metabolic syndrome have insulin resistance.
It should be noted that the prevalence of pre-diabetes and metabolic syndrome overlap but not exactly. One can consider metabolic syndrome as a pre-diabetic state. When comparing individuals without metabolic syndrome, those with this syndrome have an approximately 5-fold increase in diabetes risk. Once pre-diabetes is combined with metabolic syndrome, the risk is increased even more for diabetes.
The major adverse outcomes in individuals with pre-diabetes are macrovascular disease and type 2 diabetes, the leading contributors to microvascular disease. The macrovascular disease occurs both before and after the onset of diabetes, whereas microvascular disease occurs predominately several years after becoming diabetic. Metabolic Syndrome is a risk factor for macrovascular disease. Initial management is lifestyle intervention including:
- weight reduction
- reduced intake of dietary saturated and trans-fatty acids
- lowering cholesterol, and sodium
- increased physical activity
According to Dr. Steven Reisman, the Director of the New York Cardiac Diagnostic Center and a cardiologist in New York City these initial steps of lifestyle intervention in first-line management should be emphasized to this group of individuals along with a thorough assessment of cardiovascular risk.
Dr. Steven Reisman is an internationally recognized cardiologist and heart specialist. He is a member of the American College of Cardiology, American Heart Association, and a founding member of the American Society of Nuclear Cardiology.
Dr. Reisman has presented original research findings for the early detection of "high risk" heart disease and severe coronary artery disease at the annual meetings of both the American College of Cardiology and the American Heart Association. Dr. Reisman was part of a group of doctors with the Food and Drug Administration who evaluated the dipyridamole thallium testing technique before the FDA approved it.
Dr. Steven Reisman's academic appointments include Assistant Professor of Medicine at the University of California and Assistant Professor at SUNY. Hospital appointments include the Director of Nuclear Cardiology at the Long Island College Hospital.